Hormonal Optimization for Optimal Fat Loss
Hormones act as chemical messengers in human body. They support almost all physiological functions, such as primary drivers of metabolism, appetite, and fullness. Several hormones also significantly affect body weight due to their connection to appetite. One can take measures to maintain healthy levels of specific hormones, such as leptin, oestrogen and cortisol for a positive impact on your weight. In this article we explore the hormones that could have an impact on your weight, along with advice for maintaining appropriate levels of each.
How can hormones optimize fat loss?
The only way we can lose body fat is to create an energy deficit, and we create an energy deficit by either increasing our energy expenditure, decreasing our appetite or for a given energy deficit, we want to have some type of re-composition effect where we’re losing more fat and less lean mass for the exact same amount of weight loss. Thus, for hormonal optimization to aid fat loss, it must do one of three things:
- Increase energy expenditure
- Tissue re-composition i.e. for a given energy deficit, it maintains more lean mass and results in more fat loss, even though the weight loss is the same.
- Increased fat loss and improved LBM (Lean Body Mass) retention for given weight loss
- Decrease appetite
Which Hormones Do We Optimize?
Hormones involved in fat metabolism that may affect weight are listed below with the mechanism how does a particular hormone affect weight loss. One important thing to note here is that all these hormones interact, and sometimes when you change one another one changes. For example, insulin and ghrelin have a relationship, when insulin levels go up, it tends to suppress ghrelin. So, we can’t necessarily even isolate any single hormone by making at least dietary changes.
- Leptin (energy expenditure, appetite) – Leptin affects energy expenditure, also affects appetite.
- Insulin (appetite, recomposition) – Insulin can affect appetite. It may also possibly have an effect on tissue recomposition, because insulin not only affects fat metabolism but also impacts protein metabolism as well.
- Thyroid (energy expenditure)
- Ghrelin (appetite)
- Cortisol (appetite, recomposition) – Cortisol can affect appetite. It can also affect tissue recomposition because it can affect muscle proteolysis the breakdown of muscle protein.
- Growth Hormone (recomposition) – Growth hormone has anabolic effects and also has effects on fat metabolism, so there’s a possible recomposition effect there.
- Testosterone (recomposition) – Testosterone may also have a recomposition effect. We know that with, for example, testosterone replacement studies, when you give aging men, testosterone replacement tends to increase their fat free mass and decreases their fat mass even without any training. We also know that when it comes to anabolic steroids, which are super physiological doses of testosterone or testosterone derivatives.
- Estrogen (recomposition) – Estrogen also affects recomposition, especially fat metabolism. There’s interesting paper out there that demonstrates that part of the effects of testosterone on body fat are actually due to the conversion of testosterone into estrogen, which then affects body fat.
- Glucagon (recomposition) – Glucagon hormone produced by liver effects gluconeogenesis, which then indirectly affects protein metabolism, depending on your dietary status with your fasting resulting in a recomposition effect.
- Cholycystokinin (appetite) –
- Adiponectin (energy expenditure) – A hormone produced by fat cells just like leptin is, and adiponectin may actually impact energy expenditure.
- Glucagon-Like Peptide 1 (appetite) – Glucagon like peptide 1, GLP1 is produced by small intestine and helps regulate appetite. In fact, there’s a number of diabetes drugs that are essentially analogous of GLP1 because it also affects insulin release and so some pretty effective diabetes drugs have been developed off this hormone.
- Peptide YY (appetite) – Peptide is another hormone that impacts appetite. It is produced by intestine, feeds back on your brain, tells you that you feel more full.
There are more, for example catecholamines (a chemical that is made by nerve cells and used to send signals to other cells), epinephrine (a hormone and neurotransmitter used to treat allergic reactions, to restore cardiac rhythm, and to control mucosal congestion). Those will also have an impact on fat metabolism. We listed the above just to show to you that this is very complicated. Which one of these hormones do we optimize?
Is Optimization Even Possible?
Multiple pathways regulate feeding behaviour
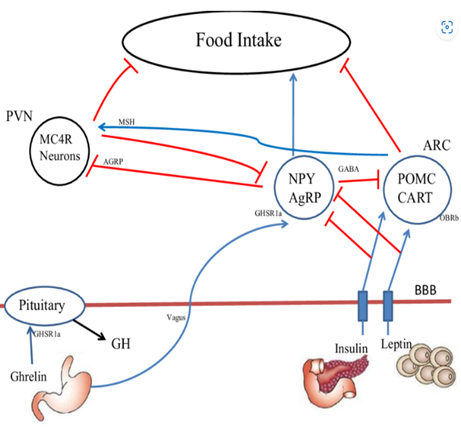
There are several different pathways that regulate our feeding behaviour. We’ve got all kinds of signals feeding back on our brain that help regulate how much we eat. There are signals from fat tissue itself. And all feedback on various areas of brain also causes changes in chemicals in brain, like neuropeptide Y or Agouti-Related Protein (AgRP), a powerful orexigenic peptide that increases food intake when administered centrally. We also got signals coming from our GI tract, which have effects on nerves and also feedback on the brain.
[A simplified diagram of the regulation of feeding behaviour at the level of the brain source]
Why is a very effective anti-obesity medication yet to be developed? The thing is that if I have to develop an anti-obesity medication, I’m going to find some or one of these pathways I can target that regulates our feeding behaviour. Now just because I inhibit or affect one pathway, look at all the other pathways that are basically redundant and take over. That’s why it is so difficult to develop an anti-obesity medication. If you affect one pathway, you still got all these other redundant pathways that you have got to worry about. And that’s why anti-obesity medications tend to have fairly poor results. When you look at randomized controlled trials on them, they may, you know, cause a few pounds of weight loss, that’s all. Just too many pathways that take over if you block one.
Multiple pathways regulate physical activity energy expenditure
Take a look at the multiple pathways in the diagram below.
This also is really complicated. There are various signals, all going every which way. It’s like a maze and so which pathway do you target if you’re trying to bump your energy expenditure up? So that’s why this brings up the question, is it even possible to optimize hormones?
What are the major hormones that are involved in fat metabolism?
Though “Hormonal optimization” for fat loss is difficult due to wide variety of hormones involved in body weight regulation, understanding the effect of some of the major hormones that are involved in fat metabolism is beneficial. The major hormones involved in fat metabolism that we talk about below are Insulin, Leptin, Ghrelin, and Cortisol. We also discuss impact of whey protein, stress and sleep on hormones and fat loss.
Insulin
The pancreas produces insulin, which is the primary hormone used for storage in body. Insulin encourages the storage of glucose, a simple sugar obtained from food, in the muscle, liver, and fat cells for later use in healthy humans. Basically, in a very simplistic term, as insulin levels go up, you get more fat and as insulin levels go down, you lose fat. Insulin has a strong effect on fat metabolism.
Why Optimizing Insulin Might Work?
Insulin inhibits lipolysis and fat oxidation. Lipolysis is the release of fatty acids from fat tissue. When Insulin levels are up, fatty acid oxidation is inhibited, lipolysis is inhibited. Intuitively, it makes sense why that might help. Therefore, the question is whether lower levels enhance fat loss? Insulin also inhibits muscle protein breakdown, so lower levels may not necessarily be beneficial. However, insulin suppresses appetite.
You control people’s diet, make them eat the same number of calories, put one on high carb, put the other one on low carb, because carb is one of the main macro nutrients that impacts insulin levels and then you look at what happens to body fat if you keep protein the same? It’s a very simple hypothesis to test, and it’s actually been tested many times. There was research where they put people in a metabolic ward and gave them low carb or high carb diets and looked at their body fat loss. What they did here is simply compared low carb and high carb diets. They found insulin levels much lower on the low carb diet versus high carb diet but the change in body fat was the same. So that would tell you that manipulating insulin levels as long as you keep protein intake the same and everything else doesn’t really matter when it comes to fat loss.
Also, it has been observed in people with diabetes, insufficient insulin prevents the body from getting glucose from the blood into the body’s cells to use as energy. When this occurs, the body starts burning fat and muscle for energy, causing a reduction in overall body weight.
What is the impact of Insulin on Hunger?
Some people call insulin, a hunger hormone. Insulin as mentioned before, suppresses appetite, so you might think, maybe if I eat foods that are more insulinemic, it may actually help with my appetite regulation. Also, there’s another hormone called Amylin, which is usually co-secreted by the pancreas along with insulin, which also will suppress food intake.
You eat food, your insulin level goes up, it tells your brain ‘Oh, I’ve eaten food now I feel satiated’. That’s the way it actually does work. Why does it not work as well in overweight individuals? It’s because one can have insulin resistance in the brain, then his insulin signal doesn’t get into the brain as well, which then may actually cause some appetite dysregulation. People who are overweight and obese, a lot of them will have insulin resistance in the brain. That’s not the insulin levels causing the problem. It’s the fact that the signals are not getting through. What’s interesting is if you look at studies there’s actually a positive relationship between insulinemia and feelings of satiety, which means with higher insulin levels you feel fuller. Higher insulin levels are correlated with less food intake 2 hours after a meal.
A note on exercise. This is why actually exercise can really help with weight loss. Even though exercise alone may not help when you don’t change diet. If you just do exercise, you may not lose a lot of fat. You really have to decrease your calorie intake to really get effective fat loss. But one of the things that exercise will do, because exercise enhances insulin sensitivity, that will also have the same impact on the brain, it will actually improve your ability to physiologically regulate your appetite, physically active people have better appetite regulation than sedentary people do.
Can we use insulinemic foods to our benefit to enhance satiety?
There’s some data that suggests that maybe. Insulinemic is the presence of an abnormally high concentration of insulin.
Insulinemic Proteins and Satiety
Someone would actually think well, maybe if I consume foods that are more insulinemic, maybe it actually might help with my appetite regulation, especially in terms of protein because you know, we all think of carbohydrates as stimulating insulin release, but a lot of people don’t realize that protein stimulates insulin secretion as well. And, some proteins are more insulinemic, particularly dairy proteins.
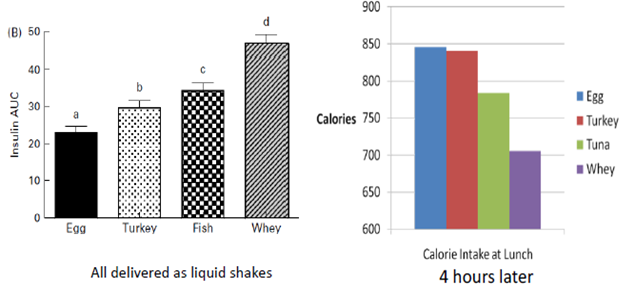
There’s one study that was really interesting. The researchers gave people different types of protein, but they delivered them as liquid shakes. What they showed was that insulin secretion increased with these different proteins, especially with whey protein.
The graph above shows how much higher insulin secretion was with whey protein compared to the other proteins. The researchers had the people eat a lunch 4 hours later. They found calorie intake was much lower after the whey protein intake compared to the other proteins. So, they suggested that perhaps the insulinemic effects of the whey had appetite suppressant effects.
What are the Positive Effects of Whey on Appetite-Related Hormones?
Studies show higher CCK, GLP-1, and GIP release compared to casein, although not observed in all studies. Postprandial hormone responses don’t always translate to satiety – casting doubt as to whether optimizing hormones matters in terms of satiety.
There is evidence that some of the satiating effects of whey are mediated through peptide YY.
A number of studies have shown that whey protein does have positive effects on appetite related hormones, not just insulin, but others also.
Some of the whey related studies show the following:
- High Whey Yogurt Reduces Ad Libitum Calorie Intake, Possibly Through Ghrelin Suppression
- Differences in Hormones May Not Matter on Hunger When Protein Intake Is High
- Even if There Are Differences in Hormones & Self-Reported Hunger Levels, It May Not Matter In Regards to Energy Intake at a Subsequent Meal
- Impact of Whey Depends Upon Timing
- Impact of Whey Protein May Be Strongest When Consumed With Or Soon Before A meal
- Whey Protein Consumed at Or immediately Around Meals Improves Fat Loss Over Soy Protein
What is the effect of dairy protein?
When one consumes more dairy protein with energy restriction, it actually slightly enhances fat loss. Note that the biggest effect with dairy protein and whey protein seems to be helpful when people are actually in an energy deficit.
Remember, if something is going to optimize hormones, you would expect a tissue recomposition effect. And this is where dairy protein seems to actually have a positive effect, it seems to actually enhance lean mass slightly.
- Dairy Enhances Fat Loss During Energy Restriction
- Dairy Improves Lean Mass, With or Without Energy Restriction
- Dairy also possibly impacts muscle protein synthesis because dairy is very high in amino acid leucine, which is essentially the primary branch chain amino acid that controls muscle protein synthesis. So that may be another way that dairy seems to help.
Summary: Optimizing Insulin for Fat Loss
Changing insulin levels, through carb manipulation, for a given energy deficit does not impact fat loss or body composition
Use of whey protein, and dairy proteins in general, at or near meals may enhance fat loss and body composition via:
- Appetite suppression
- Possibly through insulin, and/or other hormones like ghrelin, CCK, and GLP-1
- Enhanced lean mass
- Possible mechanisms include insulin and impacts of dairy on muscle protein synthesis due to high leucine content
Ghrelin
Ghrelin is a gut hormone which activates its receptor. Ghrelin’s hallmark functions are its stimulatory effects on food intake, fat deposition and growth hormone release. Ghrelin is famously known as the “hunger hormone”.
Ghrelin is an orexigenic hormone that can increase body weight. Its circulating levels increase before meals and are suppressed after food ingestion. Understanding the effects of specific types of ingested macronutrients on ghrelin regulation could facilitate the design of weight-reducing diets.
How can I affect ghrelin levels which will then impact my appetite?
An interesting study was done where they gave people different meals that contained 80% of any one of the three macro nutrients. So, it was either 80% protein, 80% carbs or 80% fat. And what they found is protein, as you might expect, actually resulted in the greatest ghrelin suppression. Not surprising. We know that protein is the most satiating macronutrient. You might want to guess what came in second. Carbs, yes, carbs came in second. Superior suppression in the short term, at least in the three hours after meal, but not less than three hours after the meal, but not more than three hours after the meal.
What was interesting though, is they did appetite ratings here, so again this is one of those cases where just cause you see differences in hormones doesn’t mean it always translated into benefits and appetite.
With Meals consisting of 80% of each macronutrient, following were the findings:
- Protein resulted in greatest overall ghrelin suppression
- Carbohydrate resulted in superior ghrelin suppression in short term (<3 h after meal), but not long term (3+ h)
- Fat had lowest ghrelin suppression
- No differences in appetite were observed
In another study, just comparing fat and carbohydrate what they found was that ghrelin suppressed way more with a 77% carb compared to 75% fat. You might have heard that one has to eat more fat to feel more satiated. Now the data doesn’t really support that, at least when it comes to added fats. Carbohydrate is pretty much in almost all studies has been found to be the more satiating macronutrient compared to fat. Hunger levels were lower with the high carb conditions, so data shows that carbohydrate is more satiating than fat is.
For this study, following were the findings:
- Ghrelin was suppressed more with a 77% carb meal compared to 75% fat
- Ghrelin was associated with hunger levels
While a few studies show greater ghrelin suppression with higher protein in meals, most do not.
Let’s summarize macronutrient composition and its impacts on ghrelin suppression. High carb meals do a better job of suppressing ghrelin more than high fat meals. That partly explains why fat is the least satiating macronutrient of all three. Now we all know that protein is the most satiating macronutrient. But there are other mechanisms behind how protein is satiating. High fat, low protein dieting approaches have been very popular in the past few years but are probably not going to be ideal for long term adherence, both from a hormonal perspective, it does not have the ideal impact on hormones that regulate appetite and this from a dietary flexibility standpoint.
Leptin
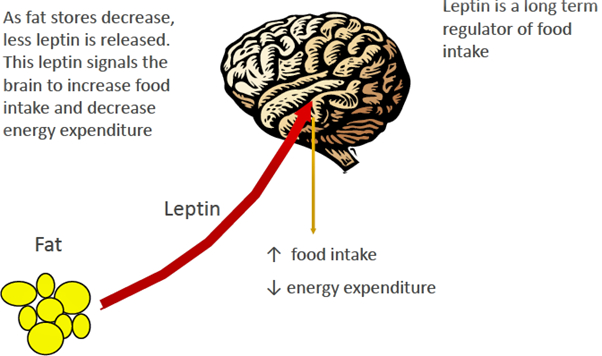
Leptin is a hormone that your adipose tissue (body fat) releases to help your body maintain your normal weight on a long-term basis. It does this by regulating hunger by providing the sensation of satiety (feeling full).
When it comes to regulating body fat, Leptin out of all the hormones is really probably the most influential hormone. When we think of a thermostat which controls the temperature in our house, what a thermostat does is if the temperature gets too hot, it will cause the air conditioning to turn on to bring the temperature down. If it gets too cold, it will kick the heat on to bring temperature back up into a certain range. Leptin acts in a similar fashion, when body fat gets too big Leptin is meant to get you to eat less. When body fat gets too small, leptin goes down, tells you, hey, we got to bring body fat levels back up.
Leptin, long-term regulator, is produced by fat cells. As fat cells grow, as they increase, they produce more leptin. This feeds back on brain. This causes a decrease in food intake, an increase in energy expenditure, which drives body fat down.
That’s how it’s supposed to work. Unfortunately, it doesn’t work very well in today’s obesogenic environment. It also works in the opposite fashion when body fat stores go down your fat cells shrink, they produce less leptin. Now since you don’t have as much leptin feeding back on the brain, you’re going to feel hungrier and it’s going to drive your appetite up. You’re going to want to eat more. This impact of leptin is very strong. This is why one of the reasons why people have a hell of a time keeping their weight off long term because of that reduced leptin signal.
Optimizing Leptin through Refeeds and Diet Breaks
Refeed is the periodic controlled intake of excess calories usually in the form of carbohydrates typically to improve weight loss during dieting. dieters using refeeds to lose extra weight.
Refeed is the short-term (1-3 day) periods in which calorie intake is increased to a maintenance level or slightly above maintenance level, usually by increasing carbohydrate intake while holding protein and fat at the same level. Dieters use refeeds to lose extra weight.
Following are the Rationale Behind Refeeds.
- Increase leptin levels to try to mitigate adaptive thermogenesis and decrease appetite
- Carbs are used because leptin levels are increased more after carbohydrate intake compared to fat intake
- Increasing calorie intake to maintenance or slightly above maintenance prevents fat gain when the body is in a metabolically efficient state where it will regain fat easily
Leptin Responds to Changes in Energy Balance.
There is evidence to Support Refeeds for Leptin Optimization. Short-term, 3-day changes in energy balance cause changes in leptin even when fat stores haven’t changed much.
- 3-days overfeeding: ↑ leptin
- 3-days underfeeding: ↓ leptin
Evidence Against Refeeds for Leptin Optimization
In studies it has been found that the increase in leptin achieved by carb overfeeding is much smaller than the increase in leptin achieved by injection.
| Leptin Injection | Carb Overfeeding | |
| Leptin Before (ng/ml) | 16.8 | 9.8 |
| Leptin After (ng/ml) | 24.8 | 12.5 |
| Leptin (ng/ml) ↑ | 8 | 2.7 |
Overfeeding carbs by 670 calories above maintenance only boosted energy expenditure by 139 calories per day
- Net surplus of 531 calories, so increase in EE was not beneficial!
- Overfeeding carbs is not the same as returning to maintenance
- The change in energy expenditure was not related to changes in leptin levels (r2 = 0.038)
Study has also found that refeeding doesn’t restore Leptin levels. Following quote are from the study:
“We find that the altered leptin levels resulting from overfeeding and underfeeding were not restored to baseline when the participants were returned to a eucaloric (in which the number of calories consumed (as food) is approximately the same as the number expended) diet.”
“Leptin levels returned to baseline only after the participants crossed over to the complementary dietary treatment and repaid the deficit or surfeit in cumulative energy balance.”
- Consistent with concept that leptin is a long-term regulator of food intake, and drives body back to original state (settling point)
- You can’t trick your body
Summary: Optimizing Leptin for Fat Loss
- Weight of the evidence indicates that changing leptin levels through refeeds will not mitigate adaptive thermogenesis.
- Leptin will not be restored to baseline levels until the cumulative energy deficit is restored (i.e., weight is regained).
- Refeeds may slightly decrease weight-loss induced appetite, perhaps through temporal increases in leptin
- The effect is likely small
- Appetite will still be strongly elevated above baseline levels if cumulative energy deficit is not restored
- Best way to lose weight? Don’t gain it in the first place
- The strong counterregulatory effects of lower leptin levels also mean that, when “bulking”, it’s best to use a slow approach with minimal fat gain
- Otherwise, subsequent fat loss efforts will be met with strong counter-regulatory signals
- The strong counterregulatory effects of lower leptin levels also mean that, when “bulking”, it’s best to use a slow approach with minimal fat gain
Cortisol
Cortisol, the primary stress hormone, increases sugars (glucose) in the bloodstream, helps burn fat into energy, enhances brain’s use of glucose and increases the availability of substances that repair tissues. Cortisol also curbs functions that would be nonessential or harmful in a fight-or-flight situation.
Cortisol stimulates fat and carbohydrate metabolism, creating a surge of energy in body. While this process is essential for survival situations, it also increases appetite. Additionally, elevated cortisol levels can cause cravings for sweet, fatty and salty foods.
Minnesota Starvation Experiment
The study was divided into four phases: A twelve-week baseline control phase; a 24-week starvation phase, causing each participant to lose an average of 25% of his pre-starvation body weight; and 2 recovery phases, in which various rehabilitative diets were tried. The first rehabilitative stage was restricted by eating 2,000–3,000 calories a day. The second rehab phase was unrestricted letting the subjects eat as much food as they would like.
- 34 conscientious participants from WWII
- ~1560 kcal/d diet (~1600 kcal/d deficit)
- 24 weeks – starvation phase
- 12-week rehabilitation period – recovery phase
- Subjects divided into groups and given one of 4 different caloric energy levels to help recover body weight
- 8-week unrestricted rehabilitation period – recovery phase
- Calorie intake and food content were unrestricted
The result found that the weight losses followed the desired pattern very closely on the average but individuals developed more pronounced irregularities and variations as edema became more prominent. The rehab phase proved to be psychologically the hardest phase for most of the men with extreme effects including self-mutilation, where one subject, Sam Legg, amputated three fingers of his hand with an axe, though the subject was unsure if he had done so intentionally or accidentally.[6]
Participants exhibited a preoccupation with food, both during the starvation period and the rehabilitation phase. Sexual interest was drastically reduced, and the volunteers showed signs of social withdrawal and isolation. The participants reported a decline in concentration, comprehension and judgment capabilities, although the standardized tests administered showed no actual signs of diminished capacity.
There were marked declines in physiological processes indicative of decreases in each subject’s basal metabolic rate (the energy required by the body in a state of rest), reflected in reduced body temperature, respiration and heart rate. Some of the subjects exhibited edema in their extremities, presumably due to decreased levels of plasma proteins given that the body’s ability to construct key proteins like albumin is based on available energy sources.
Could stress of dieting increase cortisol, and increase fluid retention?
- Increasing carbohydrate and calories would theoretically decrease cortisol and cause “whoosh” effect
- Refeed or diet breaks could potentially decrease cortisol and enhance short-term weight loss through fluid excretion
- Would lead to enhanced adherence due to improved impacts on psychology
Does Carbohydrate Feeding Reduce Cortisol?
There is inconsistent evidence, But Most Studies Say Probably Not.
- Low carb diet reduced the free testosterone/cortisol ratio in athletes
- Low carb diet resulted in higher urinary cortisol levels compared to higher carb diets
- Cortisol increased on a low carb diet in resistance trained men after 5 days, although returned to baseline after 10 days
- High carb food decreased cortisol response to stress in stress-prone people, but not low-stress people
- No effect of different levels of carb intake on cortisol in sedentary men
- No effect of carb beverage on post-resistance exercise cortisol
- No significant difference in cortisol levels between a high carb and moderate carb diet, whether at maintenance or in a deficit
- No significant difference in cortisol levels between a high carb and very low carb diet
What is the evidence against refeeds for cortisol optimization?
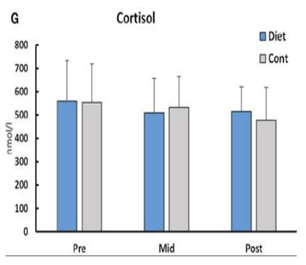
In a study of Intermittent Fasting / Energy Restriction and Fat Loss, no change was found in cortisol in dieting female fitness competitors.
It was observed that fasting elevates cortisol, but evidence indicates that dieting does not.
Stress Management and Cortisol
5 out of 8 studies showed decreases in cortisol with mindfulness-based stress reduction programs
Summary: Refeeds for Cortisol Optimization
- Weight of the evidence indicates that cortisol does not increase with dieting
- Most studies show that increasing carbohydrate intake does not decrease cortisol
- The concept of “cortisol-induced fluid retention” and flushing of fluid retention with refeeds/diet breaks is not supported by most of the evidence
- The edema observed in the Minnesota Starvation Experiment may be due to other factors
- Results of the MSE may not apply to real life situations due to the extreme nature (~1500 kcal/d deficit in non-obese individuals for 6 months)
- The edema observed in the Minnesota Starvation Experiment may be due to other factors
Stress, Hormones, and Appetite
- Primate research shows relationship between stress, cortisol, and calorie intake of hyperpalatable, energy dense foods
- Human research suggests relationship between cortisol response to stress, and hyperpalatable food intake and cravings, although data is not consistent
- Cortisol response and failure to suppress ghrelin may be related, but data is not consistent
- Unknown whether cortisol and ghrelin are causal in these relationships
- Stress management techniques and programs may reduce cortisol response to stress
- Reduced cortisol response may lead to reduced cravings and hyperpalatable food intake, assuming cortisol is causal
Sleep, Hormones & Fat Loss
Sleep Loss Increases Calorie Intake: Hormones? Maybe Cortisol.
- One small study of 12 normal weight men showed increased ghrelin and decreased leptin with sleep deprivation.
- One study showed no effect on leptin or ghrelin, but an impact on GLP-1 and insulin
- One study showed small increase in leptin with 5 days of 5.5 h sleep
- Cortisol was elevated in afternoon and evening (when it usually declines)
- No changes in appetite ratings
- No impact of sleep loss in study of 11 subjects with access to highly palatable food
- Mechanism may be increased opportunity to snack
Summary: Sleep, Hormones & Fat Loss
- Sleep deprivation leads to increased calorie intake
- Mechanism may be hormonal, but data is not consistent
- Mechanism may simply be increased opportunity for snacking
- Optimizing sleep will optimize fat loss, regardless of whether mechanism is hormonal
Conclusion
“Hormonal optimization” for fat loss is difficult due to wide variety of hormones involved in body weight regulation. Even if some hormones are optimized through various strategies, it may not make a difference in regards to outcomes in some situations (like intermittent dieting strategies)
Insulin
- Manipulating insulin levels via carbohydrate manipulation doesn’t impact fat loss for a given energy deficit
- Consumption of more insulinemic proteins (dairy, esp. whey) may enhance fat loss through appetite suppression, and also enhance lean mass retention
Ghrelin
- High fat intakes do not suppress ghrelin as much as lower fat intakes and are not as satiating
- Very high fat, low carb approaches may not be ideal due to impacts on ghrelin, and due to challenges in long-term adherence
Leptin
- Changing leptin levels through refeeds will not mitigate adaptive thermogenesis
- Leptin will not be restored to baseline levels until the cumulative energy deficit is restored (i.e., weight is regained)
- Slow approaches for bulking are best to help prevent strong counterregulatory signals when one diets
- Refeeds may slightly decrease weight-loss induced appetite, perhaps through temporal increases in leptin
- Appetite will still be strongly elevated above baseline
- Intermittent dieting strategies don’t result in superior fat loss to continuous strategies, indicating any effects on leptin have no practical significance
- Anecdotal reports of benefits of refeeds and diet breaks are likely psychological rather than physiological and due to enhanced adherence
Cortisol
- Dieting does not increase cortisol, and refeeds will not reduce it
- There may be relationships between stress, cortisol, and intake of hyperpalatable, energy dense foods
- Stress management techniques may reduce cortisol and subsequently the intake of these foods
Sleep
- Sleep loss leads to increased calorie intake
- Mechanism may be hormonal, or may simply be due to increased opportunity to snack
- Regardless of mechanism, enhancing sleep will enhance fat loss results through better control of calorie intake
Please contact me Abhinav Malhotra to learn what I and my team AbhiFit can do for you through personal training and nutrition services. We train kids, teens, adults, elders, athletes and models in Dubai and online across the UAE and around the world. We help our clients achieve their fat loss, weight loss, muscle gain, strength gain, rehab, figure / physique transformation & healthy living goals.
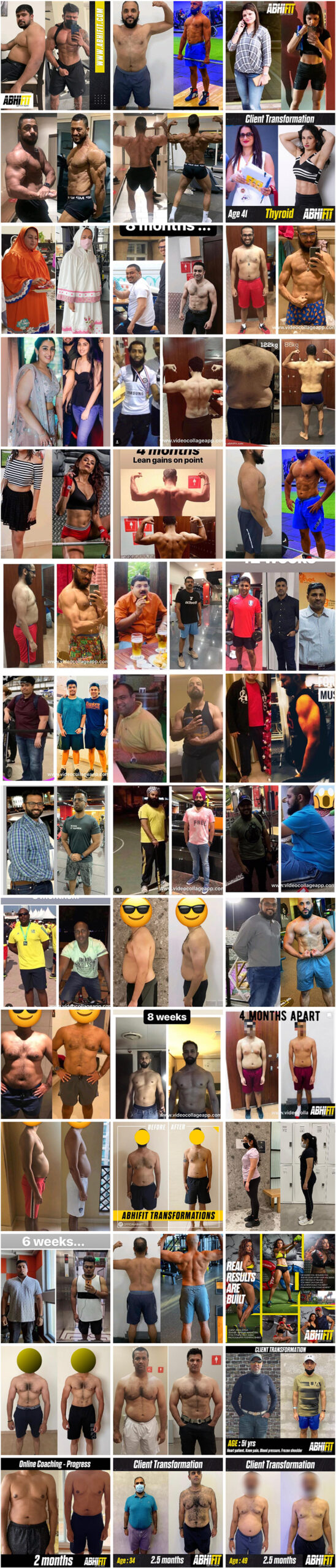
Many female and male clients including kids, teens, adults and elderly people have greatly benefited from Abhinav’s strong experience as the best personal trainer and nutritionist in Dubai, UAE. You can see some of our client transformations here here.
Email your Name and WhatsApp No. to info@abhifit.com if you want to receive a notification whenever we publish a new article.
Get Fit Now!

About Author
Abhinav Malhotra
Abhinav Malhotra is an award-winning personal trainer, coach and sports nutritionist in Dubai, UAE. He also offers online services to clients around the world. A personal trainer par excellence, Abhi has worked with the world’s leading fitness chains, supplement brands and founded his own fitness academy in India. He has achieved successes for many clients from all backgrounds and has trained the Indian Army Rugby Team. He is the first International Kettlebell Sport athlete from India.