Inflammation – What It Is and What Do We Need To Know?
- Understanding inflammation
- Understanding the inflammatory process
- Nutrition-related inflammatory disorders
- Dietary modulation of low-grade inflammation
- Obesity and chronic low grade inflammation
What is Inflammation?
Inflammation is a complex biological response of body tissues to some form of harmful stimuli. That stimuli could be pathogens, bacteria, cell damage or some kind of irritant. Inflammation is an essential part of body’s healing process. It occurs when inflammatory cells travel to the place of an injury or foreign body like bacteria. It is a part of innate immunity or non-specific immune response.
Two Different Types of Immunity
- Innate Immunity – Immunity that is present at birth and lasts a person’s entire life. Innate immunity is the first response of the body’s immune system to a harmful foreign substance. When foreign substances, such as bacteria or viruses, enter the body, certain cells in the immune system can quickly respond and try to destroy them.
- Acquired Immunity – A type of immunity that develops when a person’s immune system responds to a foreign substance or microorganism, or that occurs after a person receives antibodies from another source. For example, if you go get a vaccine that’s acquired immunity. What we’re doing is we are introducing an antigen to the body but it’s like a weakened form of the antigen or perhaps like a little part of it getting body to produce an antibody response to that antigen and now body has acquired immunity to that antigen that’s how vaccines work.
A nonspecific immune response is just a general immune response to any type of antigen that happens and inflammation is one of those responses and we’re all born with innate immunity and then we acquire immunity over time.
There’s a reason for example why do kids probably get sick a lot but as they get older and older, they get sick less and less, that’s acquired immunity. It’s because the more antigens you’re exposed to over a lifetime you just develop more and more antibodies to various antigens. But nonspecific immunity is something that everyone’s born with.
Inflammatory process
Inflammatory process is a complex process. The goal of inflammation is to respond to the stimuli and restore balance. Often, this includes eliminating the cause of tissue injury, clearing out necrotic or dead cells, and starting tissue repair.
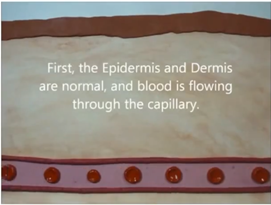
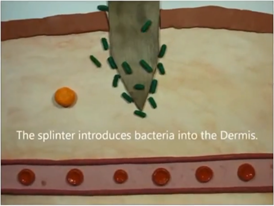
What happens is that you got a blood vessel and there is the capillary, the blood is flowing normally. Then there’s a splinter.
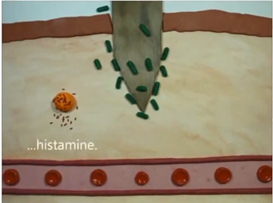
You get bacteria, now that’s gotten into the wound because it came from the splinter. Now you have what’s called a mast cell, a type of white blood cell that is found in connective tissues all through the body, especially under the skin, near blood vessels and lymph vessels, in nerves, and in the lungs and intestines. The mast cell releases histamine.
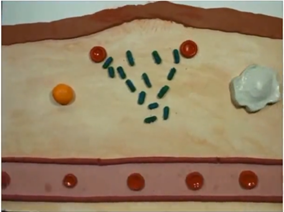
The histamine is for the capillaries to dilate, this actually opens up basically holes essentially in the capillary, which allow proteins to go into the dermis.
That’s how you get that dilation. That’s actually what’s causing that swelling and redness is that dilation of capillaries.
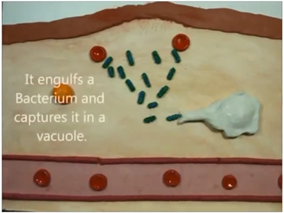
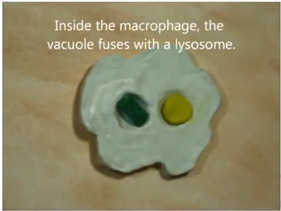
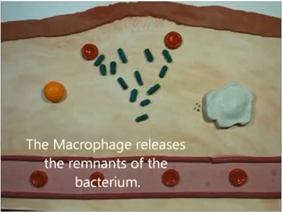
Then, you got a macrophage which is a white blood cell, it’s activated by all the proteins that are released and it actually starts to engulf the bacteria that’s a nonspecific immune response and it just basically spits out the parts of the bacteria and they say it does that until all the bacteria is destroyed and then the inflammatory response goes away.
So that’s how acute inflammation works, but it’s actually a very complicated process.
Types of Inflammation
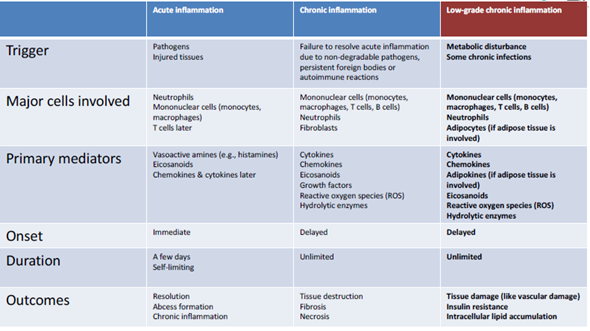
We have three major types of inflammation.
- Acute Inflammation – Acute inflammation is what we saw just above and that’s normal information, that’s actually a good thing, there’s a reason why we have that response.
- Chronic Inflammation – Chronic inflammation is where this acute information fails to resolve and this is where we can get tissue destruction and things like that. is also referred to as slow, long-term inflammation lasting for prolonged periods of several months to years. Generally, the extent and effects of chronic inflammation vary with the cause of the injury and the ability of the body to repair and overcome the damage.
- Low Grade Chronic Inflammation – This is associated with a lot of the diseases like cardiovascular disease and like that. It is defined by the persistent presence of elevated levels of circulating cytokines. This is the type of inflammation that is modulated by nutrition primarily. We will discuss this in more detail.
Inflammation: Friend and Foe
Inflammation is both a friend and a foe. Inflammation is an essential immune response that seeks to contain microbial infection and repair damaged tissue. However, inflammation may also have undesirable consequences, including potentially exacerbating tissue damage and diverting nutrients away from productive purposes. Inflammation becomes bad when it is chronic.
- Friend
- Essential part of immunosurveillance
- Important in defence against toxic agents
- Necessary component of tissue repair and healing
- Foe
- Chronic low-grade inflammation associated with:
- Metabolic syndrome
- Non-alcoholic fatty liver disease
- Type 2 diabetes
- Cardiovascular disease
- Alzheimer’s/dementia
- Chronic low-grade inflammation associated with:
Nutrition-Related Inflammatory Disorders
There are several inflammatory disorders related to nutrition.
- Cardiovascular disease – It is actually an inflammatory condition.
- Celiac disease – Celiac disease is an autoimmune disorder that’s triggered when you eat gluten.
- Inflammatory bowel disease
- Crohn’s disease
- Colitis
- Low grade systemic inflammation
- The process of low-grade systemic inflammation is the same as tissue inflammation but it’s not confined to any particular tissue,
- Widely observed in obesity
Cardiovascular disease
First you have LDL deposit on the arterial wall and then what happens is that LDL oxidises and you get macrophages infiltration into that tissue and then it produces what’s called foam cells and that’s kind of starts the whole inflammatory process of atherosclerosis – an inflammatory disease of the wall of large- and medium-sized arteries that is precipitated by elevated levels of low-density lipoprotein (LDL) cholesterol in the blood.
The Risk Factors
- Smoking
- High cholesterol
- High LDL
- Inactivity
- Hypertension
- Menopause
- Psychological stress
Celiac Disease
Celiac disease is also an inflammatory disorder. What it does is actually affects the small intestine mucosa, there’s mucus in intestine just like there is in nose. It is an immune reaction to eating gluten, a protein found in wheat, barley and rye.
Why gluten aggravates people with celiac disease? Over time, the immune reaction to eating gluten creates inflammation that damages the small intestine’s lining, leading to medical complications. It also prevents absorption of some nutrients (malabsorption).
When you actually consume gluten it’s deaminated by an enzyme called TTG and then that deaminated gluten is basically taken up by what are called antigen presenting cells, which are part of your immune system APC’s. And then these antigen presenting cells will present components of the deaminated gluten and then you get what are called activated T cells, which are also part of your immune system. Those activated T cells will then influence B cells, which are your memory cells, those are the cells that are responsible for example when you get a vaccination, basically you get responsive B cells to produce antibodies to whatever you’ve been vaccinated against. Well unfortunate here with someone with celiac disease that activation of B cells they are not getting antibodies to gluten, they are basically mounting an immune response to gluten. So, they are getting mucosal damage and all the symptoms associated with celiac disease.
To give you an idea of the prevalence of celiac disease, with all the people complaining about gluten and everything you would think prevalence would be much higher, but it’s actually very low rate. Your talking .7 to 2% of the Caucasians that actually have it and in fact East Asian populations, African populations have almost no celiac disease. So it’s very rare.
The classic symptom is diarrhoea. Other symptoms include bloating, wind, fatigue, low blood count (anaemia) and osteoporosis. Many people have no symptoms.
Symptoms
- Malabsorption
- Diarrhoea
- Abdominal pain
- Vitamin & mineral deficiencies
- Iron-deficiency anaemia
- Osteoporosis
- Growth delay
- Skin lesions
- Neurological disorders
The mainstay of treatment is a strict gluten-free diet that can help manage symptoms and promote intestinal healing.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a term for two conditions (Crohn’s disease and ulcerative colitis) that are characterized by chronic inflammation of the gastrointestinal (GI) tract.
All sort of colitis only impacts the large bowel. And it’s located in colonic mucosa. And the main clinical features is bloody diarrhoea.
Crohn’s disease is characterized by periods of remission and relapse. It can affect any part of GI tract? But typically impacts the terminal ileum and caecum, which is kind of the part of your small intestine and also the beginning of your large intestine. It’s characteristics are recurrent episodes of abdominal pain, diarrhoea, malnutrition, and anaemia.
Both Crohn’s and ulcerative colitis are associated with a 5-fold increased risk of colon cancer.
- Prevalence
- Crohn’s 50 – 100 per 100,000
- Ulcerative colitis 100-200 per 100,000
- Usually starts early in life with greatest onset between 15-25 yrs
- Disease mainly associated with industrialised countries in northern hemisphere
Risk Factors
- Genetics (especially Crohn’s)
- Western-style diet
- Smoking (Crohn’s)
- Stress
- Childhood illness
Considerable evidence that gut microbiome is involved in IBD
- Germ-free animals do not get IBD. Rodents that have no intestinal bacteria at all they do not get inflammatory bowel disease.
- Germ-free mice with genetic susceptibility to IBD only get it when repopulated with bacteria
- Ulcerative colitis patients have increased levels of mucosal IgG against colonic bacteria, and increased antibody production against anaerobic bacteria
- It’s been found that Crohn’s patients have low numbers of good bacteria. Crohn’s patients have low numbers of bifidobacterial (“good” bacteria) and higher numbers of bacteroides and peptostreptococci (A more “pro-inflammatory” phenotype of microbiome)
Gut and Inflammation
There’s still a lot we don’t know about the microbiome.
It does play a role in a number of diseases, especially intestinal diseases. But people have implicated microbiome in all kinds of things like obesity and everything else. I will say the evidence for the microbiome, actually, being a causal role in obesity is probably almost none. There’s been recent research that suggests that it’s not a causal, it’s more of a correlational thing. When people become obese, their microbiome tends to change, but the change in the microbiome is not causing the obesity, even though some people have speculated it in the past.
Basically, what we’re talking about here is gastrointestinal tract, which plays a very important role in the immune function. Gastrointestinal tract is a barrier for bad bacteria getting into blood. It’s keeping bacteria out of blood. It’s helping keep viruses out of blood. So, it plays a very big role in the immune system in inflammation. It guards against pathogen embedded invasion, maintains the gut barrier integrity. If you got more of the bad bacteria then that increases the permeability of your gut barrier to what we’d call Lipopolysaccharides or LPS.
Gut-Systemic Inflammatory Associations
Interactions between gastrointestinal tract and gut bacteria influence immune function and inflammation
- Promote development & maintenance of mucosal immune system
- Protect against pathogen invasion
- Maintain gastrointestinal tract barrier integrity
Higher gram negative (“bad”) bacteria, and lower bifidobacteria (“good”), increase gut permeability to lipopolysaccharides (LPS)
- Leads to low grade endotoxemia and inflammation
Anti-Inflammatory Benefits of Fermentable Fiber
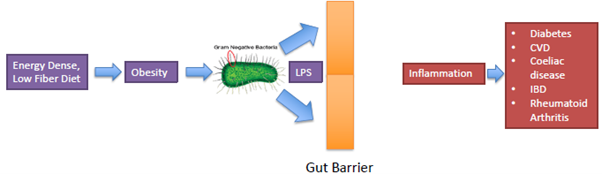
If you eat a very calorie dense low fibre diet, which then leads to obesity, which is then associated with an increase in the gram-negative bacteria, the bad bacteria that actually leads to a leaky gut. This means that your gut barrier function is not working as well and so now you can get lipopolysaccharides actually cross from the gut into the bloodstream, which then leads to an inflammatory response.
We call that kind of a low grade endotoxemia. And then that’s associated with a bunch of diseases. So, if a low fibre diet is contributing to this, well maybe eating a lot of fermentable fibre might actually have a certain anti-inflammatory benefit.
So, if you eat fermentable fibre, what that does? It actually helps with the good bacteria. And these good bacteria produce what we call short chain fatty acids. Butyrate is kind of the main one. But also got acetate and also propionate. And these short chain fatty acids, these fuel cells, which are the cells of your small intestine or say in your colon is very, very important. It acts as a barrier and so these short chain fatty acids will actually tend to stimulate mucosal production by the epithelial cells, which are the cells aligning intestinal tract. And also increases the proliferation of those epithelial cells. So, you get more cells you know. They’re increasing in number, so what that does is a couple different things. First, it decreases intestinal permeability, which is a good thing. And also decreases what we call pro inflammatory cytokines.
Experimental animal models of inflammation have shown decreased inflammation and improved outcomes with prebiotic fibre supplementation. So, there is a potential benefit to prebiotic fibre and having a high intake of it. At least from animal models, it seems that would suggest that it has a benefit. So, it really comes out brings out to this concept of.
Dietary Modulation of Low-Grade Inflammation
Can we modulate inflammation with our diet? We suggest that we can. And if we can what type of dietary components actually do modulate inflammation? One thing I’m going to show you is there are a number of dietary components that actually have been shown to modulate some of the biomarkers of inflammation, but that doesn’t necessarily mean it actually makes any difference in terms of disease outcomes or disease risk. Which things do seem to make an impact? That’s ultimately what we care about, right? We care about risk, disease, risk for disease, and also disease progression. So, what I’m going to show you is what dietary components have been found to actually improved risk of disease, and what are the ones that just show changes in biomarkers of inflammation, but don’t seem to impact risk of disease?
Many foods, nutrients, and non-nutrient food components modulate inflammation both acutely and chronically. However, there’s a lot of limitations in this research.
- Research limitations
- Measurement of small number of blood markers of inflammation, often in the fasting state
- May not necessarily reflect inflammation in tissue compartments
- May not reflect what happens in response to inflammatory challenges
Dietary Fats and Inflammation
So, let’s talk about some of the dietary components and how they might affect inflammation. OK, let’s talk about dietary fats.
Dietary fatty acids may affect inflammatory processes in two ways
- Impact on body weight and adipose tissue
- Impact on cell membrane and lipid raft composition and function
Impact on body weight and adipose tissue
- Increased energy density
- Least satiating of three macronutrients
- Most efficient macronutrient for storage as body fat (98-99%)
There are two ways that dietary fatty acids might affect inflammatory processes. First, it’s just through impact on body weight. Remember dietary fats are not as satiating as some other macro nutrients. So, typically when you eat a high fat diet, not including ketogenic diets in this set, typically you tend to overeat, eat more calories that increases body weight, increases body fat which then may affect inflammation. Body fat itself can be inflammatory. And then the other impact would be on, basically, your cell membranes. Cell membranes are made of fat fatty acids. There’s like we call it a lipid bilayer that surrounds every cell. Well, there’s fatty acids that make up that lipid, bilayer, and diet can actually impact the structure of that lipid bilayer.
Dietary fat is also the most efficient macronutrient for storage of body fat. This is one-way dietary fat could actually contribute to inflammation, just through the process of overeating and gaining body fat.
Are there any other impacts that dietary fat may have on inflammation? There is this LIPGENE trial. What they did is they had four different groups. One group consumed a lot of saturated fats. Second, group consumed a lot of monounsaturated fats. Then they had a low-fat diet. Then they had a low-fat diet supplemented with Omega threes. What they found was that it didn’t matter, there was no effect of the various types of diets on any markers of inflammation. Which goes totally against what some of the gurus out there will tell you that if you eat these types of fats it’ll be anti-inflammatory and stuff like that. Now there are limitations of this study. They just looked at fasting plasma markers of inflammation, may not necessarily reflect what’s going on in tissues. Also, it wasn’t a very long study and some have speculated maybe the EPA, DHS supplementations was too low ’cause there’s other EPA and DHA supplementations studies that actually do show improvements in inflammatory biomarkers.
Also, when we talk about saturated fats and there’s few studies that suggest how dietary saturated fatty acids may be pro inflammatory but evidence is not consistent. So, probably not.
And we talk about total dietary fat intake. As long as you control for calories most research shows none or only minor effects, so dietary fat overall doesn’t seem to have any real strong impact on inflammation. However, there may be some data on EPA, DHS.
Dairy
Vast majority of studies indicate dairy has either anti-inflammatory or neutral effects, based on common markers of inflammation in humans.
Carbs and Inflammation
High blood sugar, or hyperglycaemia, and the insulin resistance that often accompanies it, can be proinflammatory. Acute increases in blood glucose are associated with acute inflammatory responses.
- In normal glucose tolerant subjects, these responses are normalized within 2-3 h
- In obese with impaired glucose tolerance or type 2 diabetics, glucose-induced inflammation is stronger and lasts longer
Fructose and Inflammation
Dietary fructose, either alone or in HFCS, compared to other sugars has no impact on CRP levels, whether it’s consumed alone or as part of high fructose corn syrup. So, fructose is not inflammatory.
Gluten and Inflammation
We know gluten is bad for people with celiac. What about just normal folk? There’s one good study. They put people on a gluten free diet. It decreased what we call ex vivo Pro inflammatory cytokine production.
A gluten free diet decreases ex vivo pro-inflammatory cytokine production by blood immune cells, but also results in a significant reduction in “good” bacteria in the gut by 36-70%, which would suggest that all these people going on gluten free diets, it may actually, at least theoretically, might have a negative effect.
Grains and Inflammation
High whole grain intake leads to significant reductions in CRP, sICAM-1, serum amyloid, and sVCAM-1 compared to low intake.
If gluten was so bad, if gluten was so inflammatory you would see big elevations in CRP in people eating whole grains. Because there’s just as much gluten in whole grains as there is in refined grains but we actually see a decrease in a bio marker of inflammation when people eat whole grains.
Dietary Components with Potential Anti-Inflammatory Effects
- ω-3 fatty acids
- Effects on cell signalling and gene expression
- Potential Anti-inflammatory Effects:
- Decreased production of pro-inflammatory eicosanoids (like prostaglandin E2 or PGE2)
- Increased E- and D-series resolvins, which may exert anti-inflammatory and inflammation-resolving actions
- Reduced chemotaxis (cell migration to an inflamed area) of white blood cells
- Decreased adhesion molecule expression
- Decreased ROS
- Decreased inflammatory cytokines like TNF
- Antioxidant vitamins
- Effects on cell signalling and gene expression (vitamin E)
- Reducing production of ROS
- Plant flavonoids
- Effects on cell signalling and gene expression
- Prebiotics and probiotics
- Promotion of gut barrier function and anti-inflammatory responses
Potential Anti-Inflammatory Effects of α–Linolenic Acid
- There is Inverse relationship between α–linolenic acid intake and plasma levels of pro-inflammatory cytokines
- Controlled trials only show reductions in ex vivo production of pro-inflammatory cytokines at doses over 9g/d, and effects are more modest compared to EPA/DHA
- Reason for lack of effect of smaller doses is likely insufficient conversion to EPA
Potential Anti-Inflammatory Effects of Antioxidants: Vitamins C, E, Carotenoids
- Some cell culture and animal studies show reduced production of inflammatory cytokines and eicosanoids with antioxidant supplementation
- Some observational/association studies show inverse relationships between blood levels of antioxidants and biomarkers of inflammation
- Some intervention studies show reduced production of inflammatory cytokines and eicosanoids with antioxidant supplementation
Flavonoids: Anti-Inflammatory?
Flavonoids exert their anti-inflammatory activities by reducing the production of reactive oxygen species (ROS) and the down-regulation of several inflammatory mediators through key inhibition of signalling pathways.
- Flavonoids have anti-inflammatory effects
- Anthocyanin group, with certain soft fruits as most significant dietary source, may be most potent
- Human RCT’s are limited
- Mechanistic studies have been done in vitro at supraphysiological concentrations
- Limited data on animal models, and almost none on humans
- Low absorption (only 1% consumed is absorbed), and low concentration in biological fluids may indicate flavonoids don’t have a strong anti-inflammatory role in vivo
Fibre and Inflammation
A high-fibre diet potentially lowers inflammation by modifying both the pH and the permeability of the gut. The resultant reduction in inflammatory compounds may alter neurotransmitter concentrations to reduce symptoms of depression.
6 of 7 clinical trials showed 25-54% reductions in CRP with increased fibre consumption
- 0.014 – 0.032 g/kcal
- 28 – 64 g for a 2000 kcal/d diet
- Limitations
- Changes in CRP were observed in the presence of weight loss and modified saturated, monounsaturated, and polyunsaturated intakes
Prebiotic fibres and Inflammation
The prebiotic fibres can directly act on the gut epithelial and immune cells that leads to pro- or anti-inflammatory response. The overall findings suggest that prebiotics play a role in maintaining gut permeability and control of inflammation.
Prebiotic fibre supplementation significantly improves CRP levels, but no significant effects on IL-6 or TNF
- Significant heterogeneity in studies
- About 50% of studies reported a decrease of at least 1 inflammatory biomarker
Synbiotics and Inflammation
Synbiotics are mixtures of probiotics (helpful gut bacteria) and prebiotics (non-digestible fibres that help these bacteria grow).
Synbiotic supplementation significantly improves CRP and TNF levels, but no significant effects on IL-6
- Significant heterogeneity in studies
- About 50% of studies reported a decrease of at least 1 inflammatory biomarker
Fish Oil and CVD
A number of meta-analyses have actually shown, at least early ones, fish oil to reduce mortality in patients with cardiovascular disease. Some meta-analyses have been inconsistent, though with some supporting an effect and others not. I would say there’s enough evidence to suggest that fish oil does probably reduce risk of cardiovascular disease, but the effect is likely very small.
So this is one of those cases where the anti-inflammatory effects may actually affect disease risk. But it’s a very small effect. You know a risk ratio of, you know. .92 that’s just like an 8% reduction in risk. That’s not a huge. You’re talking an extra 8 out of every hundred people now not getting cardiovascular disease or not getting a heart attack or something. That’s not a huge amount, but it is still an effect. That’s why again, too many people overstate the effects of these things. A lot of people see fish oil is magical. It’s not. Does it have some positive benefits? Yeah, it does, but it’s not extreme as some people make it out to be now. Meta analysis is inconsistent.
Part of the problem now is because treatment for cardiovascular disease has gotten so good. That something like fish oil probably isn’t going to make much of a difference.
Statins and everything kind of minimize the effect of supplementation. And also a lot of the doses sometimes may be insufficient. You know, a lot of doses will just use 1 gram. That might not be enough. cause like I said, the confidence intervals in the ones that found no effect are still skewed towards a small benefit. And the problem is we don’t have any large primary prevention trials. What I mean by primary prevention is healthy people taking fish oil to prevent a cardiovascular event year down the road. That’s primary prevention. Now there is some ongoing trials, though. Right now, the vital trial is a primary prevention trial. They’re actually testing randomized controlled trial of almost 26,000 people of whether fish oil supplement will actually reduce risk of cardiovascular disease in the general population. I don’t know where these trials are at right now?
Fish Oil and IBD
Definitely seems to help both animal models and human studies’, definitely seems to improve symptoms of IBD.
Fish Oil and Rheumatoid Arthritis
Also seems to help in Rheumatoid arthritis. Number of studies show improvements. Both in anti-inflammatory activity or inflammatory activity and also symptoms
Fish Oil and Osteoarthritis
Not as good of evidence. Some studies on dogs show an improvement, but there’s only 6 human trials so far since 1992, and they haven’t been consistent and they’ve got a lot of problems with them.
Fish Oil and AD/Dementia
Meta analysis failed to show any benefit of fish oil to prevent dementia right now. Now there are limitations. They may not be lasting long enough. None of them lasted longer than 40 months. And also, the problem is you know Alzheimer’s related to so many other lifestyle factors that you may not be able to detect an effect by just looking at supplementation.
Fish Oil and Asthma and Psoriasis
Even though there’s anti-inflammatory effects, it doesn’t seem to affect the actual outcomes. And there’s no clear benefit on psoriasis.
Impact of Antioxidant Supplementation
Most studies on antioxidant supplementation have failed to demonstrate a benefit on inflammatory disease outcomes.
Probiotics and IBD
Definitely probiotics seem to help, although it’s dependent upon the strain. There’s a lot of different types of probiotics out there and a lot of them don’t do as well, But some depending on the strain, VSO #3 is one that’s been shown to have a lot of benefit. So, you need to get the right strain for whatever condition you’re using.
- Significant effect on Crohn’s
- Significant improvements in ulcerative colitis
- Supplement VSL#3 showed most benefits
Probiotics and IBS
- Beneficial effects on global IBS, abdominal pain, bloating, and flatulence scores.
- Risk ratio of IBS symptoms persisting was 0.79 (0.70 – 0.89).
- Which individual species and strains are most beneficial remains unclear.
Summary of effect of Dietary Components:
- Dietary components with evidence of anti-inflammatory benefits that may positively impact disease risk or progression
- ω-3 fatty acids (CVD, IBD, RA)
- Probiotics (IBS, IBD) (only certain strains like VSL#3)
- Dietary components with anti-inflammatory effects and uncertain effects on disease risk/progression
- Prebiotic fibre
- Dietary components with anti-inflammatory effects but likely no beneficial effect on disease risk/progression
- Antioxidants (small increased risk of mortality), flavonoids
Obesity and Chronic Low-Grade Inflammation
Obesity is a complex disease associated with an increase in several inflammatory markers, leading to chronic low-grade inflammation. Of multifactorial etiology, it is often used as a measurement of morbidity and mortality. There remains much unknown regarding the association between obesity and inflammation.
Chronic, low-grade inflammation is associated with a number of chronic diseases. Obesity is associated with macrophage accumulation in adipose tissue.
Fat loss is likely the number one way to reduce chronic low-grade inflammation.
Please contact me Abhinav Malhotra to learn what I and my team AbhiFit can do for you through personal training and nutrition services. We train kids, teens, adults, elders, athletes and models in Dubai and online across the UAE and around the world. We help our clients achieve their fat loss, weight loss, muscle gain, strength gain, rehab, figure / physique transformation & healthy living goals.
Many female and male clients including kids, teens, adults and elderly people have greatly benefited from Abhinav’s strong experience as the best personal trainer and nutritionist in Dubai, UAE. You can see some of our client transformations here here.
Email your Name and WhatsApp No. to info@abhifit.com if you want to receive a notification whenever we publish a new article.
Get Fit Now!
References
1. MNU link

Calories in drinks Source.
About Author
Abhinav Malhotra
Abhinav Malhotra is an award-winning personal trainer, coach and sports nutritionist in Dubai, UAE. He also offers online services to clients around the world. A personal trainer par excellence, Abhi has worked with the world’s leading fitness chains, supplement brands and founded his own fitness academy in India. He has achieved successes for many clients from all backgrounds and has trained the Indian Army Rugby Team. He is the first International Kettlebell Sport athlete from India.