Sleep and Brain Health
Sleep is an important part of our daily routine — we spend about one-third of our time sleeping. Quality sleep – and getting enough of it at the right times — is as essential for health as food and water. It is in everyone’s experience that without sleep it’s harder to concentrate and respond quickly, this is because sleep deprived brain can’t form or maintain the pathways that let one learn and create new memories.
Sleep affects almost every type of tissue and system in the body – from the brain, heart, and lungs to metabolism, immune function, mood, and disease resistance. Research shows that a chronic lack of sleep, or getting poor quality sleep, increases the risk of disorders including high blood pressure, cardiovascular disease, diabetes, depression, and obesity. In this article we talk about sleep and brain health, how our need for sleep is regulated and what happens in the brain during sleep.
Sleep is important to several brain functions, including how nerve cells (neurons) communicate with each other. In fact, brain and body stay remarkably active during sleep. Studies suggest that sleep plays a housekeeping role that removes toxins in brain that build up while one is awake.
What is Brain Health?
The brain is a complex organ and has at least three levels of functions that affect all aspects of our daily lives: interpretation of senses and control of movement; maintenance of cognitive, mental, and emotional processes; and maintenance of normal behavior and social cognition.
In 1948, WHO defined brain health as “a state of complete physical, mental, and social wellbeing and not merely the absence of disease or infirmity”. As defined by WHO brain health is the key to health, this is because the brain is the agent of all our actions and the mediator of all our experiences.
The US Centers for Disease Control and Prevention defined brain health as an ability to perform all the mental processes of cognition, including the ability to learn and judge, use language, and remember. The American Heart Association/American Stroke Association (AHA/ASA) presidential advisory defined optimal brain health as “average performance levels among all people at that age who are free of known brain or other organ system diseases in terms of decline from function levels, or as adequacy to perform all activities that the individual wishes to undertake.”
Therefore, we define brain health as preservation of optimal brain integrity and mental and cognitive function at a given age and absence of overt brain diseases that affect normal brain function.
Effect of Neurological Disorders on Brain Health
Neurological disorders may disrupt brain function and affect humans’ health. Medically, neurological disorders that cause brain dysfunction can be classified into three groups:
- Brain diseases with overt damage to brain structures, such as cerebrovascular diseases, traumatic brain injury, brain tumors, meningitis, and communication and sensory disorders
- Functional brain disorders with detectable destruction of brain connections or networks, such as neurodegenerative diseases (e.g. Parkinson’s disease, Alzheimer’s disease, and other dementias) and mental disorders (e.g. schizophrenia, depression, bipolar disorder, alcoholism, and drug abuse)
- Other brain disorders without detectable structural or functional impairment, such as migraine and sleep disorders.
These neurological disorders may have different or common effects on brain health and function. For instance, Alzheimer’s disease is the main type of dementia, with a decline in different domains of cognitive function. Mood disorders may cause dysfunction in execution, reward processing, and emotional regulations. In addition to physical disability, aphasia, gait and balance problems, and cerebrovascular diseases may lead to cognitive impairment and dementia, which are neglected by both patients and physicians.
Brain Diseases
Brain diseases come in different forms. Infections, trauma, stroke, seizures, and tumors are some of the major categories of brain diseases. However, here our subject is brain health as related to sleep.
- Alzheimer’s disease is a brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out the simplest tasks. In most people with the disease — those with the late-onset type symptoms first appear in their mid-60s.
Impaired sleep has been associated with Alzheimer’s disease. Studies suggest that sleep plays a role in clearing beta-amyloid out of the brain. Research has shown, lack of sleep has been shown to elevate brain beta-amyloid levels in mice.
When sleep is restricted to less than seven hours, the brain has less time to clear beta-amyloid away, leading to toxic levels of accumulation and raising the risk of developing Alzheimer’s.
- Parkinson’s disease is a brain disorder that leads to shaking, stiffness, and difficulty with walking, balance, and coordination. Parkinson’s symptoms usually begin gradually and get worse over time. As the disease progresses, people may have difficulty walking and talking.
Parkinson’s disease and sleep are closely connected. Most people with Parkinson’s have sleep problems at times. The disease itself may cause some issues, such as REM sleep disorder. You might also have insomnia or feel overly tired during the day.
- Sleep apnea is considered a risk factor for dementia. People with sleep apnea have been shown to have impaired memory and executive function.
A study by Monash University has found that obstructive sleep apnea (OSA) has been linked to an increased risk of dementia.
Brain and Sleep
According to new studies, chronic sleep deprivation can have a significant impact on the brain. Experts agree that good sleep is important for cognitive performance, particularly in the near term. Sleep deprivation has been shown in studies to decrease learning, cognitive performance, and reaction speed, like being inebriated but without the buzz. Sleep and memory storage are also tightly linked, according to researchers. They’re now questioning if lack of sleep plays a role in neurodegenerative illnesses and cognitive loss.
The Waking Brain and Degeneration of Brain Health
According to new studies, sleep deprivation can have a significant impact on the brain. Quality sleep, according to experts, is crucial for cognitive performance, especially in the near term. Sleep deprivation has been shown in studies to decrease learning, cognitive performance, and reaction time—like being drunk but without the buzz. Sleep and memory storage are also tightly linked, according to recent research. They’re now questioning if sleep deprivation plays a role in neurodegenerative illnesses and cognitive loss.
Dr. Spira at the Johns Hopkins Bloomberg School of Public Health discovered that shorter self-reported sleep duration and lower sleep quality were linked to a higher beta-amyloid load in recent research of 70 healthy adults. Unfortunately, researchers are unable to address the chicken-or-egg dilemma of whether sleep disturbance or beta-amyloid deposition occurs first, based on the findings of this study.
The studies raise important questions about the role of sleep in the onset and progression of cognitive disease, and the mechanisms linking sleep-wake patterns and beta-amyloid burden. Other studies may answer these questions.
The Sleeping Brain and Improved Brain Health
For millennia, scientists and philosophers have debated what our brains do while we sleep. Researchers now have substantial proof that a good night’s sleep can literally clear the mind. They discovered that the space around brain cells, known as the interstitial space, may enlarge during sleep, allowing the brain to drain out toxins that accumulate during waking hours, according to a study published in the journal Science. Proteins associated to neurodegenerative disorders, including as beta-amyloid, have been found to accumulate in the interstitial space in previous studies.
The environment has a big impact on brain cells. Toxins can disrupt nerve function and cause cell damage, therefore it’s critical to remove waste products from the interstitial space as rapidly as possible. The brain, unlike every other organ in the body, does not have a traditional lymphatic system to clear away waste products. CSF, cerebrospinal fluid, on the other hand, recirculates through the brain, mixing with interstitial fluid and eliminating toxins such beta-amyloid. This brain plumbing system may provide a solution to a problem that has perplexed brain researchers: how does the brain get rid of waste without the support of a lymphatic system?
CSF is produced in the middle of the brain,” explains Dr. Deane, research professor in the department of neurosurgery’s Center for Translational Neuro medicine at the University of Rochester Medical Center in New York. “It flows over the brain along the blood vessels, percolates through the brain tissue between cells, and then finds its way out through the venous part of the vascular system.” A bonus: in the flushing process, the brain may not only get rid of waste products but also may take up beneficial products.
These findings provide a potential link between poor quality sleep and greater cognitive impairment.
Sleep
There are two basic types of sleep: rapid eye movement (REM) sleep and non-REM sleep (which has three different stages). Each is linked to specific brain waves and neuronal activity. All individuals cycle through all stages of non-REM and REM sleep several times during a typical night, with increasingly longer, deeper REM periods occurring toward morning.
Stage 1 non-REM sleep is the changeover from wakefulness to sleep. During this short period (lasting several minutes) of relatively light sleep, heartbeat, breathing, and eye movements slow down, and muscles relax with occasional twitches. Brain waves begin to slow from their daytime wakefulness patterns.
Stage 2 non-REM sleep is a period of light sleep before one enters deeper sleep. Heartbeat and breathing slow down further, and muscles relax even further. Body temperature drops and eye movements stop. Brain wave activity slows down but is marked by brief bursts of electrical activity. One spends more of repeated sleep cycles in stage 2 sleep than in other sleep stages.
Stage 3 non-REM sleep is the period of deep sleep that you need to feel refreshed in the morning. It occurs in longer periods during the first half of the night. Your heartbeat and breathing slow to their lowest levels during sleep. Your muscles are relaxed, and it may be difficult to awaken you. Brain waves become even slower.
REM sleep first occurs about 90 minutes after falling asleep. Your eyes move rapidly from side to side behind closed eyelids. Mixed frequency brain wave activity becomes closer to that seen in wakefulness. Your breathing becomes faster and irregular, and your heart rate and blood pressure increase to near waking levels. Most of your dreaming occurs during REM sleep, although some can also occur in non-REM sleep. Your arm and leg muscles become temporarily paralyzed, which prevents you from acting out your dreams. As you age, you sleep less of your time in REM sleep. Memory consolidation most likely requires both non-REM and REM sleep.
Dreaming
Everyone dreams. We spend about 2 hours each night dreaming but may not remember most of our dreams. Its exact purpose isn’t known but dreaming may help one process emotions. Events from the day often invade our thoughts during sleep, and people suffering from stress or anxiety are more likely to have frightening dreams. Dreams can be experienced in all stages of sleep but usually are most vivid in REM sleep. Some people dream in color, while others only recall dreams in black and white.
Sleep Mechanisms
Two internal biological mechanisms – circadian rhythm and homeostasis – work together to regulate when we are awake and when we sleep.
Circadian rhythms, a natural, internal process that regulates the sleep–wake cycle and repeats roughly every 24 hours, direct a wide variety of functions from daily fluctuations in wakefulness to body temperature, metabolism, and the release of hormones. They control our timing of sleep and cause us to be sleepy at night and our tendency to wake in the morning without an alarm. Our body’s biological clock, which is based on a roughly 24-hour day, controls most circadian rhythms. Circadian rhythms synchronize with environmental cues (light, temperature) about the actual time of day, but they continue even in the absence of cues.
Sleep-wake homeostasis keeps track of our need for sleep. The homeostatic sleep drive reminds our body to sleep after a certain time and regulates sleep intensity. This sleep drive gets stronger every hour one is awake and causes us to sleep longer and more deeply after a period of sleep deprivation.
Factors Influencing Sleep
Factors that influence our sleep-wake needs include medical conditions, medications, stress, sleep environment, and what we eat and drink. Perhaps the greatest influence is the exposure to light. Specialized cells in the retinas of our eyes process light and tell the brain whether it is day or night and can advance or delay our sleep-wake cycle. Exposure to light can make it difficult to fall asleep and return to sleep when awakened.
Night shift workers often have trouble falling asleep when they go to bed and have trouble staying awake at work because their natural circadian rhythm and sleep-wake cycle is disrupted. In the case of jet lag, circadian rhythms become out of sync with the time of day when people fly to a different time zone, creating a mismatch between their internal clock and the actual clock.
Sleep and Structures within Brain
Sleep is a complex and dynamic process. Several structures within the brain are involved with sleep.
The hypothalamus, a peanut-sized structure deep inside the brain, contains groups of nerve cells that act as control centers affecting sleep and arousal.
Within the hypothalamus is the suprachiasmatic nucleus (SCN) – clusters of thousands of cells that receive information about light exposure directly from the eyes and control behavioral rhythm. Some people with damage to the SCN sleep erratically throughout the day because they are not able to match their circadian rhythms with the light-dark cycle. Most blind people maintain some ability to sense light and can modify their sleep/wake cycle.
The brain stem, at the base of the brain, communicates with the hypothalamus to control the transitions between wake and sleep. (The brain stem includes structures called the pons, medulla, and midbrain.) Sleep-promoting cells within the hypothalamus and the brain stem produce a brain chemical called GABA, which acts to reduce the activity of arousal centers in the hypothalamus and the brain stem. The brain stem (especially the pons and medulla) also plays a special role in REM sleep; it sends signals to relax muscles essential for body posture and limb movements, so that we don’t act out our dreams.
The thalamus acts as a relay for information from the senses to the cerebral cortex (the covering of the brain that interprets and processes information from short- to long-term memory). During most stages of sleep, the thalamus becomes quiet, letting you tune out the external world. But during REM sleep, the thalamus is active, sending the cortex images, sounds, and other sensations that fill our dreams.
The pineal gland, located within the brain’s two hemispheres, receives signals from the SCN and increases production of the hormone melatonin, which helps us go to sleep once the lights go down. People who have lost their sight and cannot coordinate their natural wake-sleep cycle using natural light can stabilize their sleep patterns by taking small amounts of melatonin at the same time each day. Scientists believe that peaks and valleys of melatonin over time are important for matching the body’s circadian rhythm to the external cycle of light and darkness.
The basal forebrain, near the front and bottom of the brain, also promotes sleep and wakefulness, while part of the midbrain acts as an arousal system. Release of adenosine (a chemical by-product of cellular energy consumption) from cells in the basal forebrain and probably other regions supports your sleep drive. Caffeine counteracts sleepiness by blocking the actions of adenosine.
The amygdala, an almond-shaped structure involved in processing emotions, becomes increasingly active during REM sleep.
The Role of Genes and Neurotransmitters
Chemical Signals to Sleep
Clusters of sleep-promoting neurons in many parts of the brain become more active as we get ready for bed. Nerve-signaling chemicals called neurotransmitters can “switch off” or dampen the activity of cells that signal arousal or relaxation. GABA is associated with sleep, muscle relaxation, and sedation. Norepinephrine and orexin (also called hypocretin) keep some parts of the brain active while we are awake. Other neurotransmitters that shape sleep and wakefulness include acetylcholine, histamine, adrenaline, cortisol, and serotonin.
Genes and Sleep
Genes may play a significant role in how much sleep we need. Scientists have identified several genes involved with sleep and sleep disorders, including genes that control the excitability of neurons, and “clock” genes such as Per, tim, and Cry that influence our circadian rhythms and the timing of sleep. Genome-wide association studies have identified sites on various chromosomes that increase our susceptibility to sleep disorders. Also, different genes have been identified with such sleep disorders as familial advanced sleep-phase disorder, narcolepsy, and restless legs syndrome. Some of the genes expressed in the cerebral cortex and other brain areas change their level of expression between sleep and wake. Several genetic models–including the worm, fruit fly, and zebrafish–are helping scientists to identify molecular mechanisms and genetic variants involved in normal sleep and sleep disorders. Additional research will provide better understand of inherited sleep patterns and risks of circadian and sleep disorders.
Sleep Studies
Polysomnogram is used to diagnose a sleep disorder. It typically involves spending the night at a sleep lab or sleep center. Breathing, oxygen levels, eye and limb movements, heart rate, and brain waves are recorded throughout the night. Sleep is also video, and audio recorded. The data can help a sleep specialist determine if one is reaching and proceeding properly through the various sleep stages. Results may be used to develop a treatment plan or determine if further tests are needed.
How Much Sleep Do We Need?
Our need for sleep and sleep patterns changes as we age, but this varies significantly across individuals of the same age. There is no magic “number of sleep hours” that works for everybody of the same age.
- Babies initially sleep as much as 16 to 18 hours per day, which may boost growth and development (especially of the brain).
- School-age children and teens on average need about 9.5 hours of sleep per night.
- Most adults need 7-9 hours of sleep a night.
- After age 60, nighttime sleep tends to be shorter, lighter, and interrupted by multiple awakenings. Elderly people are also more likely to take medications that interfere with sleep.
In general, people are getting less sleep than they need due to longer work hours and the availability of round-the-clock entertainment and other activities.
Many people feel they can “catch up” on missed sleep during the weekend but, depending on how sleep-deprived they are, sleeping longer on the weekends may not be adequate.
Tracking Sleep Through Smart Technology
Millions of people are using smartphone apps, bedside monitors, and wearable items (including bracelets, smart watches, and headbands) to informally collect and analyze data about their sleep. Smart technology can record sounds and movement during sleep, journal hours slept, and monitor heartbeat and respiration. Using a companion app, data from some devices can be synced to a smartphone or tablet or uploaded to a PC. Other apps and devices make white noise, produce light that stimulates melatonin production, and use gentle vibrations to help us sleep and wake.
See a doctor if you have a problem sleeping or if you feel unusually tired during the day. Most sleep disorders can be treated effectively.
Sleep is the Rx for Brain Health
In the current century, sleep deprivation is having a disastrous influence on human health, brain and mental health, life expectancy, safety, productivity, and children’s education across the world. In the last few hundred years, we humans have abandoned biologically mandated need for appropriate sleep – a requirement that evolution spent millions of years honing in service of life-support functions.
In developed countries, the silent sleep loss epidemic is the largest public health concern of the twenty-first century. A major adjustment in our personal, cultural, professional, and societal respect of sleep is required if we are to avoid the strangling noose of sleep neglect.
Sleep helps the brain re-organize itself, essentially. Brain tasks that occur during sleep include disposing of toxins that build up in the brain during the day and stabilizing memories of the day’s events. Getting enough sleep is also linked to higher levels of cognitive performance, creativity, and improved moods.
Some Ways How Sleep Helps Brain:
- Sleep helps our brain work faster and more accurately.
- Sleep helps our brain make sense of new information.
- Sleep helps our brain cement memories.
- Sleep helps our brain think more creatively.
- Sleep helps our brain clear out harmful toxins.
- Sleep helps our brain regulate our appetite.
- Sleep helps our brain keep our body looking good.
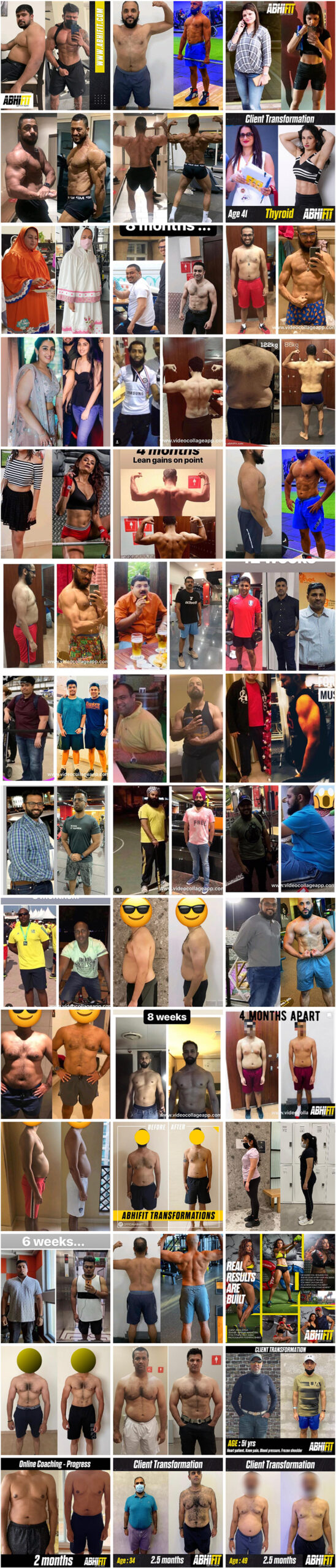
Please contact to learn what we can do through our nutrition and personal training services for kids, teens, adults, elders, athletes and models in Dubai and online across the UAE and around the world to achieve your fat loss, weight loss, muscle gain, strength gain, rehab and figure / physique transformation goals.
Many female and male clients including kids, teens, adults and elderly people have greatly benefited from Abhinav’s strong experience as the best personal trainer and nutritionist in Dubai, UAE. You can see some of our client transformations here.
Email your Name and WhatsApp No. to info@abhifit.com if you want to receive a notification whenever we publish a new article.
Get Fit Now!
Sources:
- https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep
- https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(21)00102-2/fulltext
- https://www.news-medical.net/health/The-Anatomy-of-the-Human-Brain.aspx
- https://www.forbes.com/sites/bryanrobinson/2021/02/18/these-10-sleep-habits-can-boost-brain-health-and-advance-your-career/?sh=448948e14206
- https://www.britannica.com/summary/brain
- Book: “Why We Sleep” Author: Matthew Walker

Calories in drinks Source.
About Author
Abhinav Malhotra
Abhinav Malhotra is an award-winning personal trainer, coach and sports nutritionist in Dubai, UAE. He also offers online services to clients around the world. A personal trainer par excellence, Abhi has worked with the world’s leading fitness chains, supplement brands and founded his own fitness academy in India. He has achieved successes for many clients from all backgrounds and has trained the Indian Army Rugby Team. He is the first International Kettlebell Sport athlete from India.
