
Irritable Bowel Syndrome (IBS) Causes & Treatments
Irritable Bowel Syndrome (IBS) is a chronic, relapsing and often life-long disorder characterized by the presence of abdominal pain or discomfort, which may be associated with defecation and/or accompanied by a change in bowel habit.
It is a functional gastrointestinal disorder, a group of symptoms not a disease. It includes abdominal pain / cramping, diarrhea, a change in bowel habit, bloating of abdomen, flatulence, urgent need to go to the toilet.
ROME Criteria for IBS
The Rome criteria is an international effort to create scientific data to help in the diagnosis and treatment of functional gastrointestinal disorders, such as irritable bowel syndrome. The Rome criteria have been evolving from the first set of criteria issued in 1989 (The Rome Guidelines for IBS).
Rome I Criteria for IBS (1992)
- Continuous or recurrent symptoms for at least last 3 months.
- Abdominal pain or discomfort, relieved with defecation and/or associated with change in frequency and/or consistency of stool
- An irregular (varying) pattern of defecation at least 25% of the time and two or more of following:
- Altered stool frequency (> 3 bowel movements per day or < 3 bowel movements per week)
- Altered stool form (lumpy/hard or loose/watery)
- Altered stool passage (straining or urgency, or a feeling of incomplete evacuation)
- Passage of Mucus
- Bloating or feeling of abdominal distension
Rome II Criteria for IBS (1999)
- At least 12 weeks of abdominal discomfort or pain, which need not be consecutive, in the preceding 12 months that has 2 or 3 features
- Relieved with defecation
- Onset associated with a change in frequency of stool
- Onset associated with a change in form (appearance) of stool
Rome III Criteria for IBS (2006)
- Recurrent abdominal pain or discomfort, 3 days per month in the last 3 months, associated with two or more of the following:
- Improvement with defection; and/or
- Onset associated with a change in frequency or stool; and/or
- Associated with a change in form (appearance) of stool
The Rome IV update was published 10 years later in May 2016. This covers epidemiology, pathophysiology, psychosocial and clinical features, and diagnostic evaluation and treatment recommendations for 33 adult and 17 pediatric functional gastrointestinal disorders.
NICE Guidelines
NICE (National Institute for Health and Care Excellence) published guidelines in 2008. This guideline covers diagnosing and managing irritable bowel syndrome (IBS) in people aged 18 and over. This guideline suggests the following:
- Have regular meals, take time to eat and avoid missing meals
- Drink at least 8 cups of fluid per day
- Restrict tea/coffee to 3 cups per day
- Reduce intake of alcohol and fizzy drinks
- Limit high-fiber food
- Reduce intake of resistant starch
- Limit fresh fruit to 3 portions per day
- Avoid sorbitol (for diarrhea symptoms)
- Eat oats & linseeds (for wind/bloating symptoms)
- Discourage the use of Aloe Vera
- If general advice unsuccessful, low FODMAP diet trialled under supervision from a trained professional
Diagnosis
There are no specific tests for IBS. IBS does not cause any obvious detectable abnormalities in the digestive system. IBS diagnosis is typically based on symptoms. Attempts have been made to identify specific biomarkers.
Symptoms
Despite being a heterogeneous disorder IBS symptoms typical include:
- Disordered defecation
- Constipation or diarrhea, which may be debilitating
- Abdominal distension
- Bloating
- Abdominal pain
- Non-ulcer dyspepsia or coeliac disease
Males vs. Females
- Sex ratio in IBS is highly skewed towards female gender.
- Sex hormones play a key role in IBS physiopathology
- Fluctuations in IBS symptoms during the menstrual cycle, especially exacerbation of abdominal pain at menses
- IBS patients report that their symptoms (pain, bloating, altered bowel habits) are more severe in the premenstrual period.
POTENTIAL TRIGGERS (CAUSES)
- Diet
- Caffeine
- Stress and Anxiety
- Alcohol
- SIBO
- Chronic Antibiotic Use
Diet
A low-FODMAP diet is designed to help people with irritable bowel syndrome (IBS) have better control over their symptoms by limiting certain foods. FODMAPs stands for fermentable oligo-saccharides, di-saccharides, mono-saccharides and polyols. Put more simply, FODMAPs are certain types of carbohydrates — the sugars, starches, and fiber in foods.
- oligo-saccharides – Starch, Dextrin, Cellulose, Pectin, Glycogen
- di-saccharides – Sucrose, Lactose, Maltose
- mono-saccharides – Glucose, fructose, galactose
- polyols – Sugar alcohols e.g. Sorbitol
These are Short chains of sugar molecules, easily broken down in the large intestine. Fermented rapidly by bacteria, which can contribute to gastrointestinal symptoms in sensitive individuals.
For most, these foods are not a problem unless you eat too much of them. But some people are sensitive to them. FODMAPs draw water into your digestive tract, which could make you bloated. If you eat too much of them, they can hang around in your gut and ferment.
Examples:
- Fructose: Fruits, honey, high-fructose corn syrup, agave
- Lactose: Dairy
- Fructans: Wheat, onions, garlic
- Galactans: Legumes, such as beans, lentils, and soybeans
- Polyols: Sugar alcohols and fruits that have pits or seeds, such as apples, avocados, cherries, figs, peaches, or plums
Avoiding FODMAPs doesn’t help everyone. But in a study published in the journal Gastroenterology, about 3 out of 4 people with IBS had their symptoms ease right away after starting a low-FODMAP diet and felt the most relief after 7 days or more on the plan.
A low FODMAP diet appears to be more effective than standard dietary advice for symptom control in IBS.
Resistant Starch
A type of starch that isn’t fully broken down and absorbed, but rather turned into short-chain fatty acids by intestinal bacteria
- acetate, propionate, and butyrate
Once they enter the bowel they ferment and produce gas.
Fiber Manipulation
- Treat the symptoms not IBS:
- Diarrhea – Reduce Insoluble fiber
- Wholegrain bread, bran, cereals, nuts, seeds (not golden linseeds)
- Constipation – Increase Soluble Fiber
- Oats, Barley, Rye, Fruit, Root vegetables, Golden linseeds
- Systematic review showed fiber supplementation is beneficial in mild to moderate IBS-C and Chronic Constipation
Mechanism of action of fiber on intestinal transit time and visceral hypersensitivity
*Being an MNU nutritionist in Dubai, I have taken this graphic from my MNU course lectures.
Gluten
- ’a mixture of two proteins present in cereal grains, especially wheat, which is responsible for the elastic texture of dough’
- Intolerance to gluten (celiac disease) is only prevalent in 0.5 – 1%
- Individuals may be intolerant to food containing gluten, which provides justification for improved symptoms
Gluten Sensitivity Study
- Double-blind cross-over trail of 37 subject
- 2-week diet of reduced FODMAPs, high-gluten (16 g gluten/d), low-gluten (2 g gluten/d and 14 g whey protein/d), or control (16 g whey protein/d) diets
- Results
- No evidence of specific or dose-dependent effects of gluten in patients with NCGS placed diets low in FODMAPs
- Gastrointestinal symptoms consistently and significantly improved during reduced FODMAP intake
- Gluten-specific effects shown in only 8% of participants
Caffeine
Coffee Stimulates the GI Tract
- Drinking coffee can stimulate a motor response of the distal colon in some normal people
- Caffeinated coffee stimulates colonic motor activity. 60% stronger than water and 23% stronger than decaffeinated coffee
- Coffee stimulates gallbladder contraction and colonic motor activity
- Acidity of Coffee Irritates the Intestines
- Highly acidic so stimulates the hyper secretion of gastric acid
- Coffee tends to speed up the process of gastric emptying, which may result in highly acidic stomach contents passing into the small intestines
- Drinking coffee can stimulate movement of the colonic muscles, thus promoting peristalsis
Stress and Anxiety
“An overzealous stress response may significantly alter not only the sensitivity of the central and enteric nervous systems, but also other potentially important factors such as gut motility, intestinal mucosal permeability and barrier functioning, visceral sensitivity, mucosal blood flow, immune cell reactivity and enteric micro biota composition.
Symptoms of these (mal) adaptive changes may include constipation, diarrhea, bloating and abdominal pain, manifesting clinically as IBS.”
Meditation
Significant improvements within 3 month
- Flatulence
- Belching
- Bloating
- Diarrhea
Constipation approached significance (P=0.07)
Benson’s Relaxation Response Meditation appears to be a viable treatment for IBS.
Fish Oils
- Anti-inflammatory response
- Stress
- Double-blind, placebo-controlled, randomized clinic trial
- 120 women with moderate-severe psychological distress
- 05g E-EPA/d + 0.15g E-DHA/d 8wk
- Improved significantly more with E-EPA than placebo
Exercise
- Improvement in symptoms of IBS with a more active lifestyle in males and female
- Increasing physical activity improves symptoms in randomized controlled trial
- Stimulates gastrointestinal motility, improving colonic transit time, gas transit and bloating
- Strenuous endurance training
- Diarrhea and gastrointestinal cramps
Alcohol
- Fermentation – Glucose à Alcohol & CO2
- Inhibits the absorption of sodium and water which contributes to diarrhoea
- Chronic alcohol use impairs
- Balance of micro flora in the gut
- Gut barrier function
- Liver’s ability to detoxify bacterial products
- Generate a balanced cytokine milieu
- Brain’s ability to regulate inflammation in the periphery
- Alcohol has been associated with increased abdominal pain but not IBS
SIBO (Small Intestinal Bacterial Overgrowth) – Dysbiosis
‘condition in which abnormally large numbers of bacteria are present in the small intestine, while the types of bacteria found in the small intestine are more like the bacteria found in the colon’
Most common form of dysbiosis
- Bacteria from the large intestine
- Move into the small intestines
- Where they are harmful
- And they multiply!
Microvilli Damage
- Microvilli lines the small intestine, containing sensitive carbohydrate-digesting enzymes on the tips
- They may become damaged by bacterial enzymes, toxin, inflammation and autoimmune reactions Robillar (Fast Tract Diet)
- If the structure or enzymes become damaged, digestion and the ability to absorb nutrients. This may result in mal absorption that floods the intestines with undigested food. Creating an environment where bacteria can flourish in the small intestine -> SIBO.
36 Hour Fast
- Reset the gut!
- No research but tested…
- Kanazawa and Fukudo (2006)
- Control with psychotherapy
- 10 days starvation + 5 day refeed
- 84 IBS patients
- Results
- Starvation significantly reduced: abdominal pain–discomfort, abdominal distension, diarrhea, anorexia, nausea, and anxiety and interference with life in general.
Chronic Antibiotic Use
- Diarrhea occurs in 20% of patients who receive antibiotics
- Antibiotics may directly affect the indigenous gut microbiota by compromising colonization resistance and favoring the growth of pathogenic microorganisms
- Antibiotics demonstrate significant change in the variety of bacteria strain and the development of certain pathogen
- Note: Viral infections are not affected by antibiotics, so you’re simply killing off all your beneficial gut bacteria
Antibiotics kill good bacteria & make you fat
- Obese, pre diabetic men
- 7-days of amoxicillin, vancomycin, or placebo
- Only Vancomycin decreased bacterial diversity
- Results, no effect of antibiotics on:
- tissue-specific insulin sensitivity, energy/substrate metabolism, postprandial hormones and metabolites, systemic inflammation, gut permeability, and adipocyte size
- Importantly, energy harvest, adipocyte size, and whole body insulin sensitivity were not altered at 8-week follow up, despite a still considerably altered microbial composition
TREATMENTS
Step 1: Consider what symptoms are there and discuss the potential triggers.
Step 2: Next step is to start thinking about what treatments may be most appropriate.
Step 3: Discuss, test, review, re-test
Alternative treatments
Aloe Vera
- Potential mechanism
- Reduces constipation via a Laxative for regular bowel movement
- Effect
- Double-blinded placebo study showed no benefits for IBS
Curcumin
- Potential mechanism
- Inhibits the production of inflammatory cytokines and soothing the digestive tract and decrease symptoms
- Effect
- Limited research for the effect of gut health.
Magnesium
- Potential mechanism
- Reduce constipation by acting as a laxative, exerting an osmotic effect in the lumen to increasing the fluidity of intraluminal contents
- Effect
- No research has been conducted on IBS patients with constipation
Other Alternative treatments
- Weight Loss
- Smoking Cessation
- Alcohol Avoidance
- Meal Habits
Medication
- Antispasmodics – which help reduce abdominal (stomach) pain and cramping
- Laxatives – which can help relieve constipation
- Anti motility medicines – which can help relieve Diarrhea. Anti motility agents act by modulating intestinal contractions and reducing frequency of bowel movements.
- Low-dose antidepressants – which were originally designed to treat depression, but can also help reduce stomach pain and cramping independent of any antidepressant effect
- Would need to refer – expert.
Medication is dependent on expression of symptoms which should decide the appropriate recommendations. Each symptom has a different pathology. Think from a diagnostic point of view.
Symptom Dependent Approach for Treatment
| Symptoms | Mechanism | Potential Treatment |
| Stomach Pain | Bloating/Distention,
Cramping |
Low FP diet, Stress
reduction, Fasting |
| Diarrhea | Loose frequent stool | Reduce insoluble fiber,
reduce caffeine, polyols |
| Flatulence | Excessive gas | Low FODMAP Diet, consider
Micro biota e.g. SIBO |
| Constipation | Stool remains in the colon | Hydration, Increase soluble
fiber |
| Bloating | Excessive gas | Low FODMAP Diet, consider
Micro biota e.g. SIBO |
Please contact me Abhinav to discuss and learn what I and my team AbhiFit in Dubai, UAE can do for you through nutrition and personal training if you suffer from IBS.
Please also contact me to learn about our nutrition and personal training services for kids to adults in Dubai, UAE to achieve your muscle gain, strength gain, fat loss and figure / physique transformation goals.
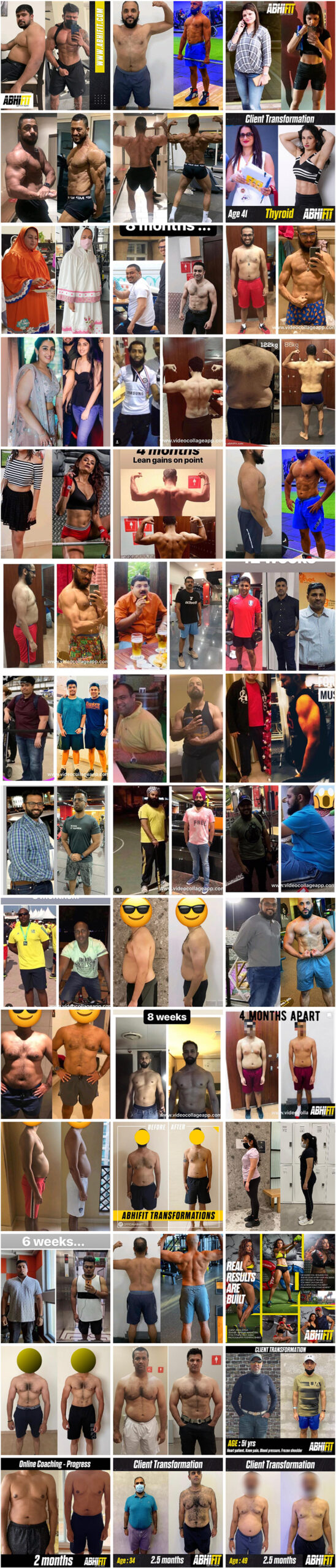
Many female and male clients including kids, teens, adults and elderly people have greatly benefited from Abhinav’s strong experience as a top personal trainer and nutritionist in Dubai, UAE. You can see some of his client transformations here.
Email your Name and WhatsApp No. to info@abhifit.com if you want to receive a notification whenever we publish a new article.
Get Fit Now!

About Author
Abhinav Malhotra
Abhinav Malhotra is an award-winning personal trainer, coach and sports nutritionist in Dubai, UAE. He also offers online services to clients around the world. A personal trainer par excellence, Abhi has worked with the world’s leading fitness chains, supplement brands and founded his own fitness academy in India. He has achieved successes for many clients from all backgrounds and has trained the Indian Army Rugby Team. He is the first International Kettlebell Sport athlete from India.

